Special Needs Parent Checklist
Track Your Progress
Use this checklist to track essential steps for supporting your child. Check items as you complete them and add notes for personal reminders.
Essential Steps
Medical
Education
Therapy
Home
Support
Finances
When you become the parent of a Special Needs Child, a child who requires additional educational, therapeutic, or medical support due to physical, cognitive, or emotional differences, the journey can feel both rewarding and overwhelming. You might wonder, is it hard to raise a special needs child? The answer isn’t a simple yes or no-it's a mix of unique challenges, valuable resources, and countless moments of joy.
What Makes the Experience Different?
Every family’s story is distinct, but most parents report three common themes: navigating specialized services, adapting daily routines, and managing emotional stress. The first hurdle often involves understanding the child's specific diagnosis-whether it’s Autism Spectrum Disorder, Down syndrome, or a less‑known condition. It’s not just the label; it’s how the diagnosis shapes communication, learning, and social interaction.
Financial considerations also surface early. Therapy sessions, specialist appointments, and adaptive equipment can add up quickly, especially if you’re relying on private providers. However, many public systems-like Ireland’s Education and Training Boards-offer funding, but the paperwork can be a maze.
Lastly, the emotional roller‑coaster affects everyone in the household. Siblings may feel neglected, partners can experience strain, and parents often grapple with guilt or self‑doubt. Recognising these pressures is the first step toward building resilience.
Core Support Systems You’ll Need
A solid foundation begins with an Individualized Education Plan (IEP), a legally binding document that tailors educational goals, accommodations, and services to a child's unique needs. In Ireland, the term is usually "Education, Health and Care Plan (EHCP)". Working closely with an Educational Psychologist, you’ll map out goals for literacy, social skills, and sensory regulation.
Therapies form the next pillar. Speech Therapy helps children develop functional communication, while Occupational Therapy focuses on fine motor skills and sensory processing. Many families also benefit from Physical Therapy when mobility challenges are present.
Don’t overlook the power of Parent Support Groups. Connecting with other families provides emotional validation, practical tips, and sometimes even shared transportation to appointments. In Dublin, the National Association for Parents of Children with Disabilities (NAPCD) runs regular meet‑ups.
Daily Strategies That Make a Difference
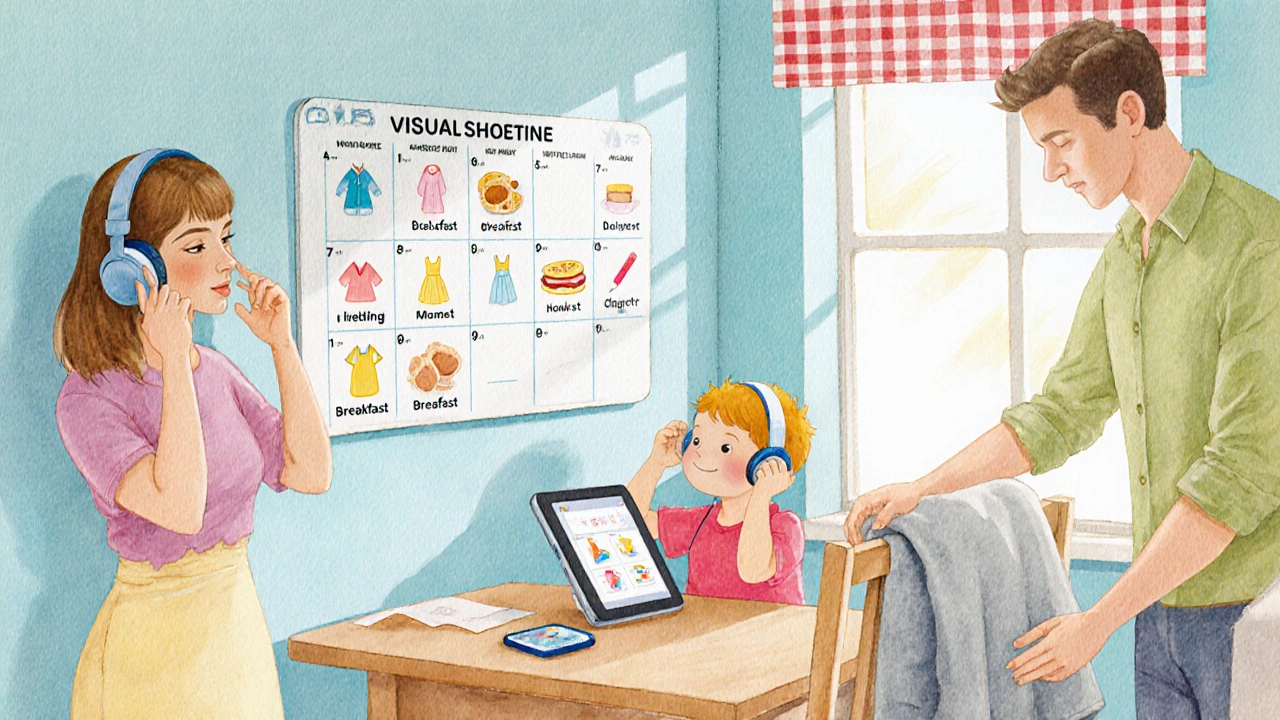
Creating predictable routines is a lifesaver. Visual schedules-using pictures or simple icons-help children understand what comes next, reducing anxiety. A typical morning might include a visual cue for dressing, breakfast, and a calm‑down corner before heading out.
Communication shortcuts matter. For non‑verbal children, augmentative and alternative communication (AAC) devices like Assistive Technology tablets can bridge the gap. Even low‑tech options such as picture exchange communication systems (PECS) work wonders when consistently used.
Behavioural challenges often stem from sensory overload. Simple tweaks-noise‑cancelling headphones, dimmer lighting, or a weighted blanket-can create a calmer environment. Pair these adjustments with positive reinforcement: celebrate small victories with stickers or extra playtime.
Nutrition and sleep are not to be ignored. Some children have selective eating patterns; working with a dietician can ensure balanced intake. Consistent bedtime routines, perhaps with a weighted lap pad, improve sleep quality, which in turn boosts daytime focus.
Building a Robust Support Network
Beyond the immediate family, you’ll want a coalition of professionals. List them in a spreadsheet: name, role, contact, and preferred communication method. This makes it easier to coordinate appointments and share updates.
Schools that practice inclusive education-where special needs students learn alongside peers-often have dedicated Inclusive Classroom teachers. These educators receive extra training in differentiation and collaborative planning, which can lighten your load.
Local charities and NGOs frequently offer free workshops on topics like “Understanding Sensory Processing” or “Navigating EHCP paperwork”. Attending these sessions not only expands your knowledge but also introduces you to potential allies.
Online communities are equally valuable. Forums such as “Special Education Ireland” on Facebook host thousands of parents sharing resources, legal advice, and real‑world experiences. Bookmark reliable sites like the Health Service Executive (HSE) and the Irish Special Education Needs Forum for up‑to‑date guidelines.
Resources and Tools Worth Exploring
Here’s a quick list of actionable resources:
- HSE’s Special Needs Services Directory - searchable by county.
- Irish Association for Special Education (IASE) - offers webinars and policy updates.
- “MyNextStep” app - tracks therapy goals, medication, and appointments.
- “Speech Buddy” - a free AAC app suitable for early communicators.
- Funding Guide by Citizens Information - step‑by‑step on applying for the Disability Allowance.
When evaluating any tool, ask: Does it align with my child’s strengths? Is it user‑friendly for me? Does it integrate with existing services? These questions keep you from over‑investing in flashy but ineffective solutions.

Quick Checklist for New Parents
| Area | Action Item | Tip |
|---|---|---|
| Medical | Secure a thorough diagnosis | Ask for a multidisciplinary report |
| Education | Apply for an IEP/EHCP | Use the school’s special‑needs liaison officer |
| Therapy | Schedule regular speech & OT sessions | Track progress in a simple spreadsheet |
| Home | Set up visual daily schedules | Reuse laminated cards for durability |
| Support | Join a parent support group | Attend monthly meetings for peer advice |
| Finances | Explore government grants | Check the Citizens Information portal quarterly |
Use this checklist as a living document-update it as your child grows and needs evolve. Remember, flexibility is your greatest ally.
Frequently Asked Questions
Frequently Asked Questions
Will my child ever be “normal”?
Every child has a unique profile. "Normal" is a moving target, but many families find that with the right supports, their child can lead a fulfilling, independent life. The goal is not to erase differences but to empower strengths.
How can I afford therapy costs?
Start with public provisions: the HSE offers funded speech and occupational therapy for eligible children. Use the Citizens Information website to identify additional grants, and consider crowd‑funding platforms for specific equipment.
What if my child resists school inclusion?
Open a dialogue with the inclusive classroom teacher and the special‑needs coordinator. Gradual exposure-starting with shorter periods and supportive peers-often eases anxiety. Adjust the IEP to include sensory breaks if needed.
How do I talk about my child’s needs with grandparents?
Use simple, factual language. Share the child’s strengths first, then explain specific supports. Offer a short brochure from the HSE so they can read at their own pace.
Is it okay to ask for help?
Absolutely. Accepting help reduces burnout and models healthy coping for your child. Whether it’s a sibling watch‑over, a friend’s ride to therapy, or a professional counsellor, each bit of support matters.
